If sexual function declines in your 40s, most men assume it’s about desire or aging. It’s usually neither. It’s circulation.
What’s failing isn’t interest. It’s blood flow, recovery capacity, and nervous system regulation. Libido doesn’t disappear on its own. It gets suppressed when the body is running in survival mode.
Sexual function is one of the first systems to degrade when cardiovascular health slips, not because sex is special, but because it’s expensive. It requires blood flow, oxygen delivery, hormonal balance, and a calm nervous system. When those are compromised, the body reallocates resources to functions that keep you alive.
This isn’t dysfunction. It’s triage.
Why Vascular Health Shows Up in Sexual Function First
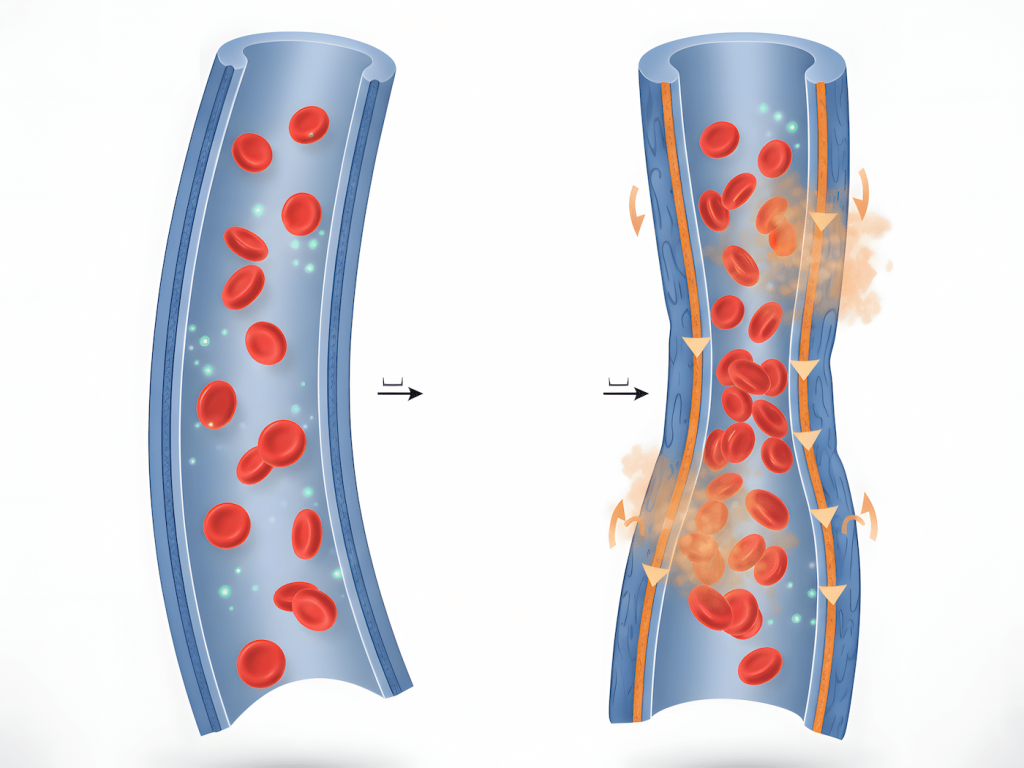
An erection is a vascular event. Arousal depends on blood flow, endothelial function, and nitric oxide signaling, the same systems that regulate blood pressure and long-term cardiovascular stability.
When circulation efficiency drops, sexual performance follows. Not eventually. Immediately.
The penis contains some of the smallest blood vessels in the body. When vascular health degrades, those vessels fail first. You won’t feel chest pain yet. You won’t have numbness in your extremities. But you will notice that arousal takes longer, erections are less reliable, and recovery between attempts extends from minutes to hours or days.
This is why sexual health often degrades years before more obvious cardiovascular warnings appear. The body is already struggling. You’re just not reading the signal correctly. You already broke down how stress drives these blood pressure patterns in how stress affects hypertension.
Calling this a libido issue is like calling engine failure a gas pedal problem.
What You’re Actually Experiencing (But Probably Dismissing)
By your 40s, the damage isn’t new. It’s cumulative.
Decades of elevated cortisol, poor sleep, vascular strain, and low-grade inflammation have compounded. Natural nitric oxide production drops with age. Endothelial cells lose elasticity. Your body was compensating for years. By the time sexual function is visibly affected, the system has been failing in the background far longer than you realize.
Here’s what that actually looks like day-to-day:
You wake up tired even after 7 or 8 hours of sleep. Not occasionally. Consistently. The fatigue isn’t dramatic, it’s just there. You assume it’s normal aging. It’s not. It’s inadequate recovery because your cardiovascular system never fully resets overnight. This is the same exhaustion pattern covered in waking up exhausted.
You need coffee to function, then need alcohol to wind down. The stimulant depressant loop becomes non-negotiable. You don’t feel like you’re “abusing” anything. You just feel like you’re managing. But both substances are directly impairing the vascular function required for sexual health.
You’re irritable more often than you used to be. Small frustrations feel bigger. You snap at your partner over things that wouldn’t have bothered you five years ago. That’s not a personality shift. It’s nervous system dysregulation.
Intimacy starts feeling like one more thing on the list. Not because attraction is gone, but because your body is running a resource deficit. Every output, including sex, requires fuel you don’t have. So the system deprioritizes it.
You rationalize all of this. “Work is stressful.” “I’m just getting older.” “I’ll rest this weekend.”
But rest doesn’t fix it. Because the problem isn’t acute fatigue. It’s systemic failure.
Why the 40s Accelerate Everything
The 40s don’t introduce new problems. They reveal accumulated damage.
In your 20s and 30s, your cardiovascular system could absorb stress, poor sleep, alcohol, stimulants, and inconsistent recovery without obvious consequences. You had vascular reserve. That reserve is now depleted.
Nitric oxide production, the molecule that dilates blood vessels and enables erections, declines naturally with age. Endothelial function degrades. Arterial stiffness increases. Add decades of lifestyle strain and what should be gradual becomes rapid.
Men don’t fail suddenly in their 40s. They run out of buffer.
The body was compensating. Now it can’t. And sexual function is the first place you notice because it’s the first system the body stops supporting when resources are tight.
Chronic stress keeps cortisol elevated. Elevated cortisol does two things that directly impair sexual function: it suppresses testosterone production and constricts blood vessels.
Testosterone isn’t just about “drive.” It’s required for nitric oxide synthesis, the molecule that enables erections. When cortisol stays high, testosterone drops, nitric oxide availability declines, and vascular tone suffers.
Add sleep debt and the damage compounds. Poor sleep reduces nitric oxide even further, raises resting blood pressure, and impairs autonomic recovery. You don’t feel “sick.” You feel tired. You wake up exhausted even after a full night because the system never fully resets.
By the time libido is affected, cardiovascular strain has usually been present for years, not weeks. The broader consequences of accumulated sleep debt are outlined in sleep debt and wellness.
Because burnout doesn’t resolve with rest alone. You can log 8-9 hours in bed and still wake up with elevated blood pressure, reduced vascular elasticity, and a nervous system stuck in high alert.
Rest helps acute fatigue. It doesn’t reverse systemic degradation. If your endothelial function is impaired, your cortisol regulation is broken, and your autonomic nervous system can’t downshift, sleeping more just gives you more time in a depleted state.
This is the same failure mode described in the burnout trap. The system doesn’t reset just because you stop working for a weekend. It requires active rebuilding of cardiovascular capacity.
Sexual readiness drops because the body avoids any output it can’t sustain. Telling yourself to “just relax” doesn’t restore blood flow. It just adds frustration to the problem.
Alcohol and caffeine are the most common coping mechanisms for stress and fatigue. Both directly impair the systems required for sexual function.
Alcohol disrupts sleep architecture even in moderate amounts. It impairs REM sleep, reduces overnight testosterone production, and damages endothelial function. You might fall asleep faster, but you don’t recover. The next day, your vascular system is more strained, not less.
Caffeine in excess raises cortisol, constricts blood vessels, and disrupts circadian rhythm when consumed too late in the day. Dependence makes everything worse. You’re not boosting performance, you’re borrowing energy from a system that’s already depleted. The pattern is covered in caffeine strategy.
Add chronic dehydration to the mix, common when caffeine and alcohol consumption are high, and vascular strain increases even further. Fatigue starts mimicking more serious circulatory and neurological issues, as explained in fatigue mimics stroke.
The system looks functional. It’s barely holding together.
For married couples, sexual health isn’t about performance metrics. It’s about whether intimacy is even on the table.
When one partner’s body is stuck in survival mode, intimacy becomes harder, not because attraction has faded or connection is gone, but because the system can’t support it consistently. This mirrors the same physiological shutdown described in survival mode.
Here’s what partners often notice first: withdrawal that looks like disinterest but is actually exhaustion. Irritability that seems disproportionate. A pattern where sex gets initiated but abandoned halfway through because the body can’t sustain arousal. Avoidance that isn’t about rejection, it’s about shame over something that used to be effortless.
The person experiencing the decline often interprets this as personal failure. The partner often interprets it as loss of desire. Neither is true. It’s cardiovascular insufficiency showing up in the most vulnerable part of the relationship.
Sexual health isn’t an individual problem. It’s a shared recovery signal. When one person’s cardiovascular system is compromised, both people feel it, not as blame, but as information about what needs support.
Fixing this isn’t about trying harder in the bedroom. It’s about rebuilding the system outside of it.
What Actually Moves the Needle (And Why Most Men Won’t Do It)
There are no hacks. No supplements that restore circulation in 30 days. No single intervention that reverses years of accumulated strain.
Cardiovascular health improves through controlled blood pressure, restorative sleep, reduced stimulant and depressant dependence, and rebuilt recovery capacity. You already broke down how recovery is rebuilt under load in recovery nutrition for weekend warriors.
Supportive nutrition plays a role, real food that improves circulation over time, not isolated supplements. Garlic, ginger, fatty fish, leafy greens, beets. The kind of eating covered in Filipino food as recovery medicine.
But here’s the problem: none of this is dramatic.
You won’t feel better in three days. You won’t see results in two weeks. The improvements are gradual, incremental, and require sustained consistency over months.
Most men won’t do it.
They’ll try a supplement. They’ll sleep more for a weekend. They’ll cut coffee for three days, feel worse, and conclude it wasn’t the problem. They’ll blame age, stress, or their partner before they’ll address the system.
The men who do fix this are the ones who stop looking for shortcuts and start treating their cardiovascular health like the foundation it is. They manage blood pressure. They sleep consistently. They reduce reliance on stimulants. They rebuild work capacity gradually instead of oscillating between depletion and overcompensation.
When circulation improves, sexual function follows. Not immediately. But reliably.
The Reframe That Actually Matters
If sexual health declines in your 40s, the question isn’t “What’s wrong with my libido?”
The question is: “What is my cardiovascular system struggling to support right now?”
Sexual function isn’t a separate system. It’s a status indicator for something much larger.
You can ignore it. Most men do. They rationalize, compensate, and avoid until the signal becomes undeniable.
Or you can treat it as the early warning it is, and fix the system before it fails in ways you can’t ignore.
Fix the system. The signal improves.

